-
Phacoemulsification in patients with diabetes: from preoperative evaluation to postoperative management
-
Yeoun Sook Chun
-
Insights Cataract Refract Surg 2025;10(3):65-75. Published online October 31, 2025
-
DOI: https://doi.org/10.63375/icrs.25.012
-
-
 Abstract Abstract
 PDF PDF ePub ePub
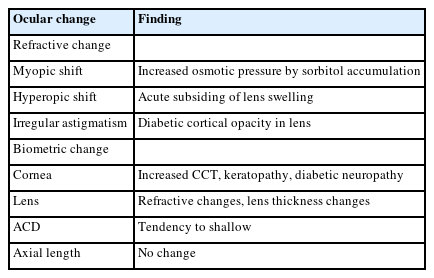
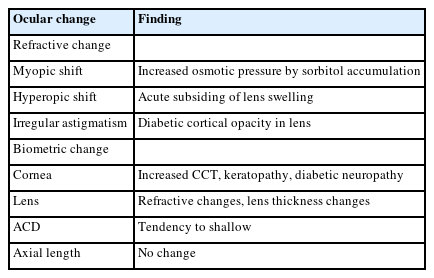
- Diabetes mellitus is one of the most common chronic diseases worldwide and is a leading cause of blindness in patients over the age of 50 years. Patients with diabetes have an elevated risk of developing cataracts compared to individuals without diabetes; furthermore, cataracts also tend to progress more rapidly in this population, leading to the need for surgery at a younger age. This review aims to summarize the key considerations in the management of cataract surgery in patients with diabetes, from preoperative evaluation to postoperative care. Patients with diabetes often present with unstable refractive status, dry eye disease, corneal epithelial defects, and recurrent corneal erosions. They also tend to have reduced corneal endothelial cell density and small pupils, both of which increase the risk of intraoperative complications. Postoperatively, these patients are at risk of developing pseudophakic cystoid macular edema, posterior capsular opacification, endophthalmitis, progression of diabetic retinopathy, and neovascular glaucoma. Patients with long-standing or poorly controlled diabetes face a higher likelihood of postoperative complications, highlighting the importance of regular ophthalmic follow-up examinations. Furthermore, adjunctive treatments such as timely intravitreal injections of anti-vascular endothelial growth factor agents may reduce the risk of vision-threatening complications following cataract surgery.
-
Trabecular microbypass using iStent combined with cataract surgery
-
Yeoun Sook Chun
-
Insights Cataract Refract Surg 2025;10(2):42-51. Published online June 30, 2025
-
DOI: https://doi.org/10.63375/icrs.25.007
-
-
 Abstract Abstract
 PDF PDF ePub ePub
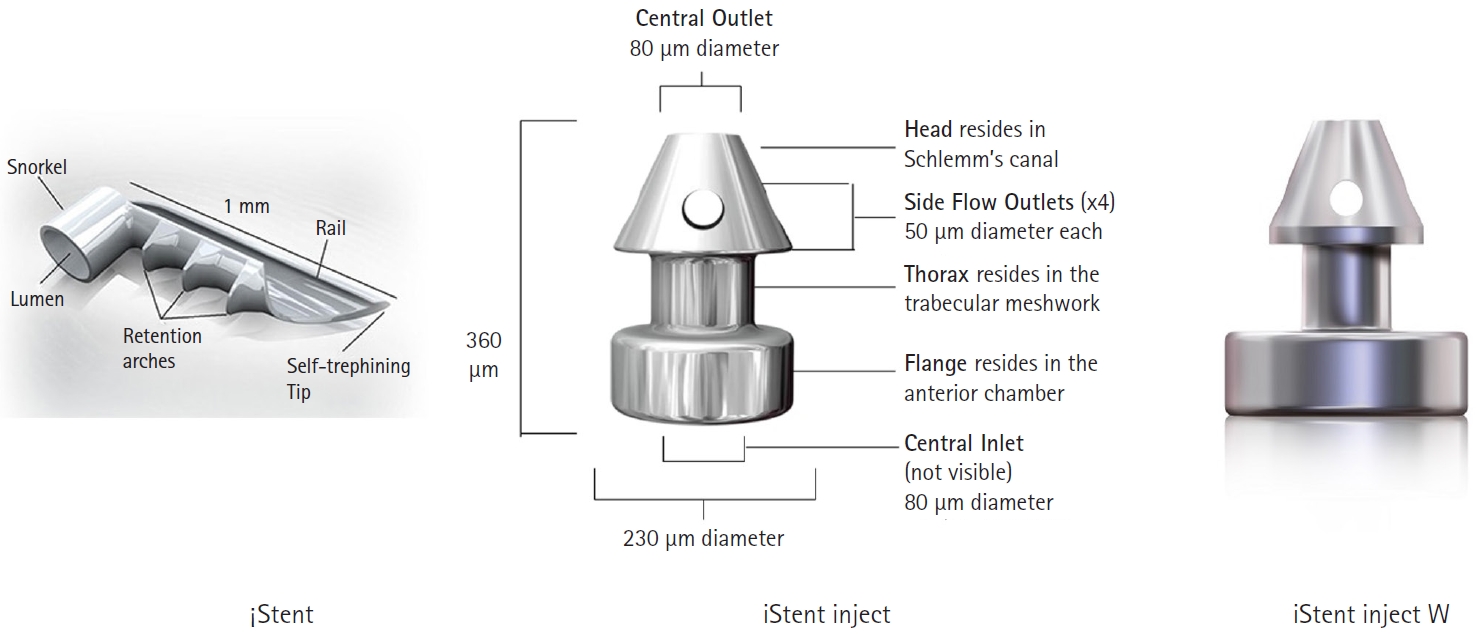
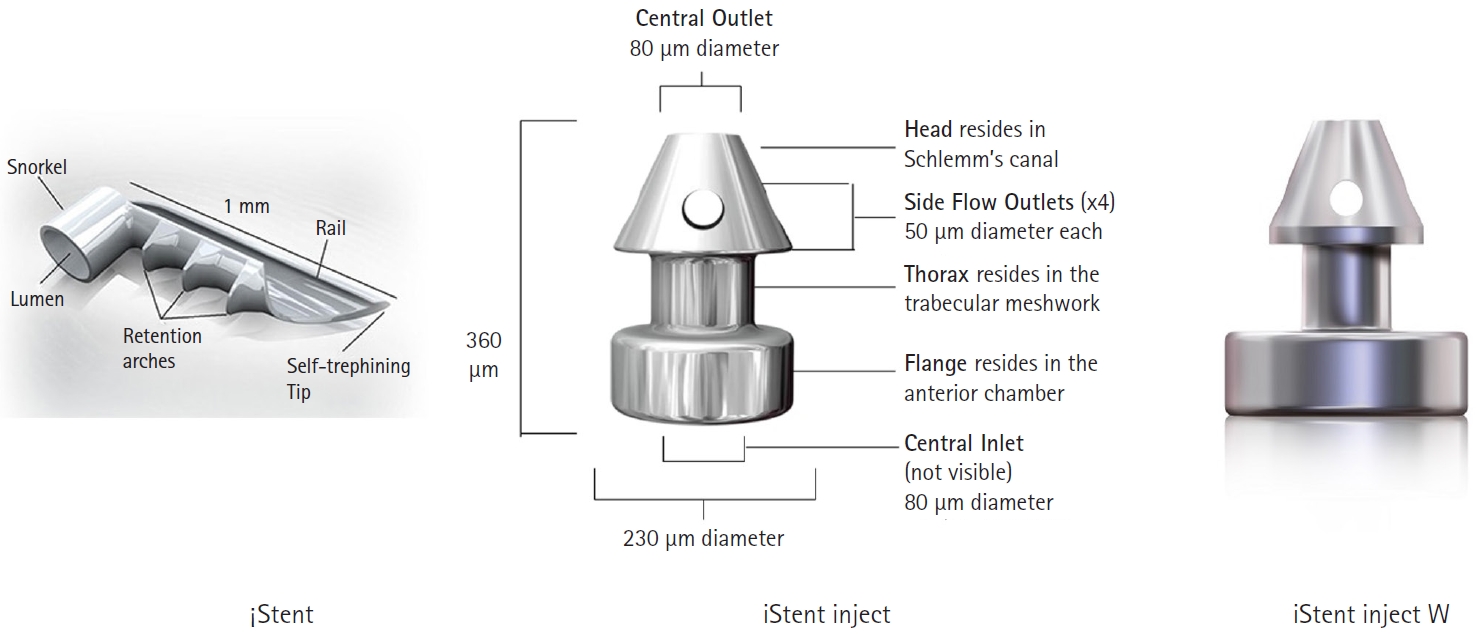
- Minimally invasive glaucoma surgery has revolutionized conventional glaucoma treatment due to its simple procedures, rapid recovery, and few complications. iStent, a trabecular microbypass that can be implanted via combined cataract surgery, has the advantage of lowering intraocular pressure (IOP) independent of bleb formation. Furthermore, it is straightforward to implement and does not involve a substantial burden. iStent has a synergetic effect with phacoemulsification. Combining iStent with phacoemulsification yielded a greater reduction of IOP and glaucoma eyedrops, as well as higher rates of visual field change, than when either modality was used in isolation. iStent has emerged as a new treatment option for patients with mild to moderate glaucoma. This review aims to improve readers’ understanding of iStent by summarizing the surgical techniques needed to correctly insert it for optimal outcomes and discussing problem-solving in the context of patient care.
-
Delayed toxic anterior segment syndrome after cataract surgery: a case report
-
Yeoun Sook Chun
-
Insights Cataract Refract Surg 2025;10(1):26-31. Published online February 28, 2025
-
DOI: https://doi.org/10.63375/icrs.25.005
-
-
 Abstract Abstract
 PDF PDF ePub ePub
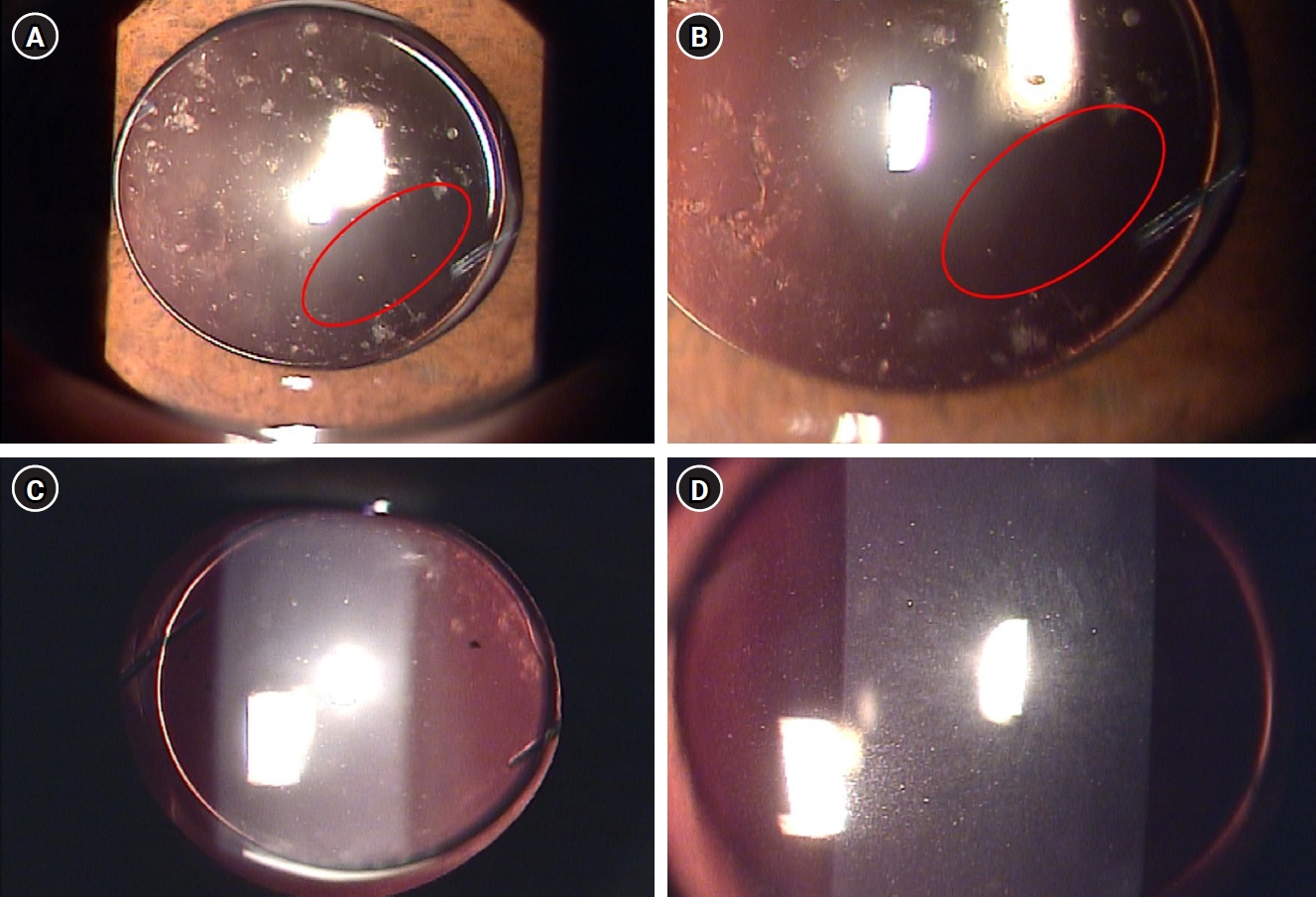
- Purpose
This report describes an unusual case of delayed toxic anterior segment syndrome (TASS) following cataract surgery and its treatment.
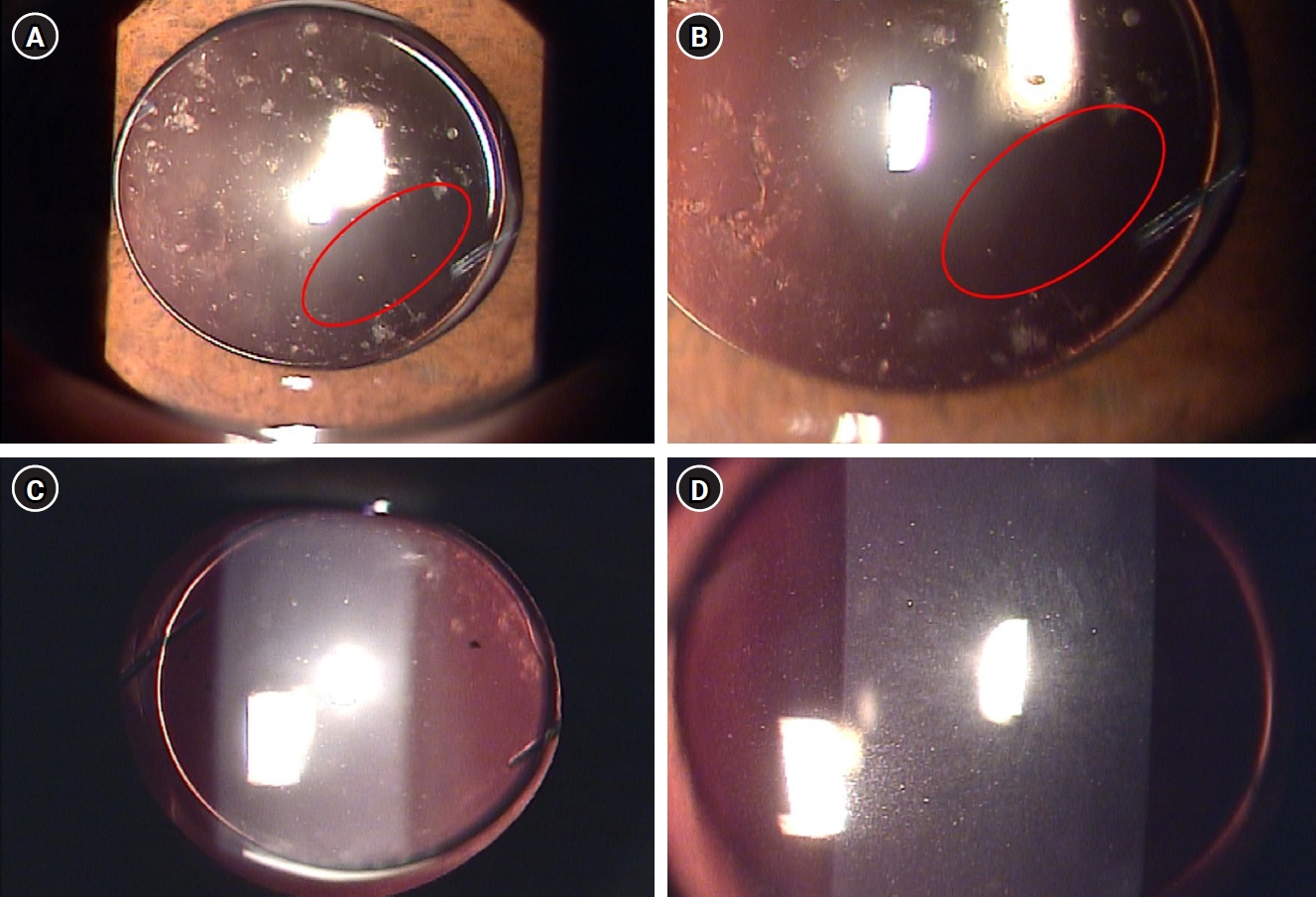
Case
summary: A 55-year-old male patient underwent uneventful phacoemulsification with implantation of an intraocular lens (IOL) and eye patching with ophthalmic ointment at the end of the operation. At 1 week postoperatively, a significant increase in the number of anterior chamber inflammatory cells and multiple gray-white deposits on the anterior surface of IOL were noted. All laboratory tests to exclude infectious endophthalmitis were negative. Under the presumptive diagnosis of delayed TASS, an intensive topical steroid was administered. The number of anterior chamber cells decreased; however, the patient complained of blurry vision and multiple whitish precipitates remained on the IOL. Neodymium:yttrium-aluminum-garnet (Nd:YAG) laser treatment was performed to disrupt and remove the precipitates. The deposits were easily and clearly removed using the laser, and there was no recurrence during a 2-year follow-up.
Conclusion
Delayed-onset TASS can manifest as lumpy white inflammatory cell deposits that cannot be controlled with topical steroids. However, Nd:YAG laser treatment can effectively remove inflammatory precipitates.
|