Previous issues
- Page Path
- HOME > Browse articles > Previous issues
Editorials
- Insights in Cataract and Refractive Surgery: a new beginning for a leap forward
- Jong Suk Song
- Insights Cataract Refract Surg 2025;10(1):1-1. Published online February 28, 2025
- DOI: https://doi.org/10.63375/icrs.25.002
- 538 View
- 12 Download

- Personal history of the silicone phakic posterior chamber intraocular lens
- Kenneth J Hoffer
- Insights Cataract Refract Surg 2025;10(1):2-6. Published online February 28, 2025
- DOI: https://doi.org/10.63375/icrs.25.001
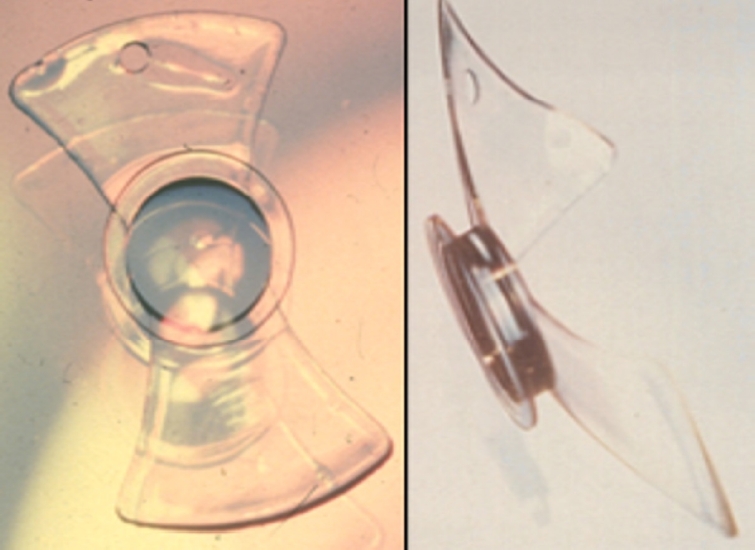
- 2,089 View
- 27 Download

Review Article
- Selection of an optimal intraocular lens according to the stage of epiretinal membrane
- Sang Beom Han
- Insights Cataract Refract Surg 2025;10(1):7-12. Published online February 28, 2025
- DOI: https://doi.org/10.63375/icrs.25.003
-
 Abstract
Abstract
 PDF
PDF ePub
ePub - Epiretinal membrane (ERM), one of the most common retinal diseases, can cause various degrees of visual disturbance, reduced contrast sensitivity, and metamorphopsia. ERM is not infrequently encountered during preoperative evaluations for cataract surgery, and selecting an appropriate intraocular lens (IOL) according to the location and stage of ERM is necessary in order to improve visual outcomes and patients’ satisfaction. This review summarizes the application of various IOLs—such as multifocal, extended depth of focus, and enhanced monofocal IOLs—in eyes with ERM, and discusses the selection of an appropriate IOL.
- 875 View
- 17 Download

Original Articles
- Visual and refractive outcomes of keratorefractive lenticule extraction using VISUMAX 800 (SMILE Pro) to correct myopia in Koreans: a 3-month follow-up study
- Sang-Mok Lee, Si-Hoon Park, Tae Keun Yoo, Jae Hyoung Park, Beom Jin Cho, Kee Yong Choi, Jong Woo Kim
- Insights Cataract Refract Surg 2025;10(1):13-18. Published online February 28, 2025
- DOI: https://doi.org/10.63375/icrs.25.004
-
 Abstract
Abstract
 PDF
PDF ePub
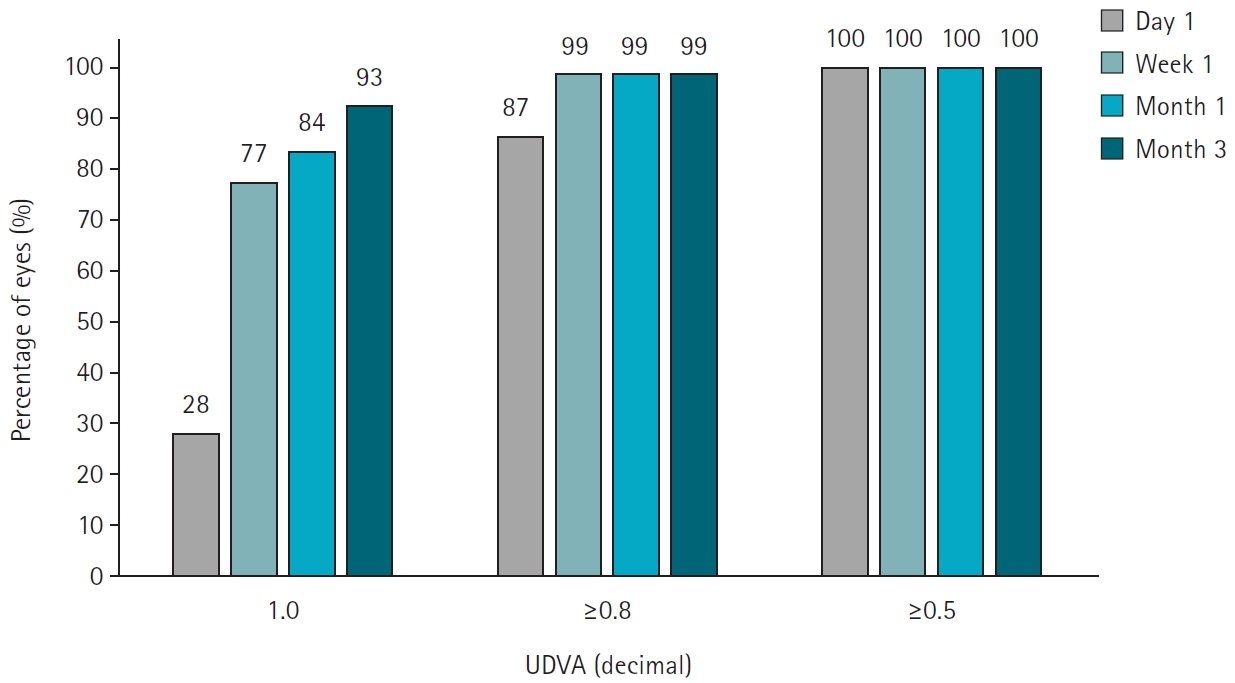
ePub - Purpose
The aim of this study was to report the clinical outcomes of SMILE Pro surgery in Korean myopia patients.
Methods
A retrospective analysis was conducted on the medical records of 90 patients (178 eyes) who underwent SMILE Pro surgery at our institution between October 2023 and June 2024 and were followed for 3 months postoperatively.
Results
Preoperative best corrected visual acuity was 0.009±0.020 (logarithm of the minimum angle of resolution). The average spherical equivalent was –5.13±2.16 diopters (range, –1.00 to –10.10 diopters), and the average astigmatism was –1.21±0.91 diopters (range, 0 to –4.0 diopters). Postoperatively, the uncorrected distance visual acuity at 1 day, 1 week, 1 month, and 3 months were 0.061±0.054, 0.013±0.027, 0.009±0.023, 0.005±0.021, respectively. At 3 months postsurgery, the predictive accuracy for spherical equivalent was 100% within ±0.5 diopters and 98.9% within ±0.25 diopters. For astigmatism, the predictive accuracy was 97.2% within ±0.25 diopters and 99.4% within ±0.5 diopters 97.2% and 99.4%. The scores for the efficacy and safety of refractive surgery at 3 months were both 1.01±0.05.
Conclusion
SMILE Pro surgery for myopia correction in Korean patients demonstrated excellent efficacy, safety, and predictive accuracy, with no significant difference compared to conventional SMILE surgery.
- 1,292 View
- 22 Download

- Clinical manifestations after cataract surgery in patients with moderate Fuchs corneal endothelial dystrophy
- Myung-Sun Song, Dong Hyun Kim
- Insights Cataract Refract Surg 2025;10(1):19-25. Published online February 28, 2025
- DOI: https://doi.org/10.63375/icrs.25.006
-
 Abstract
Abstract
 PDF
PDF ePub
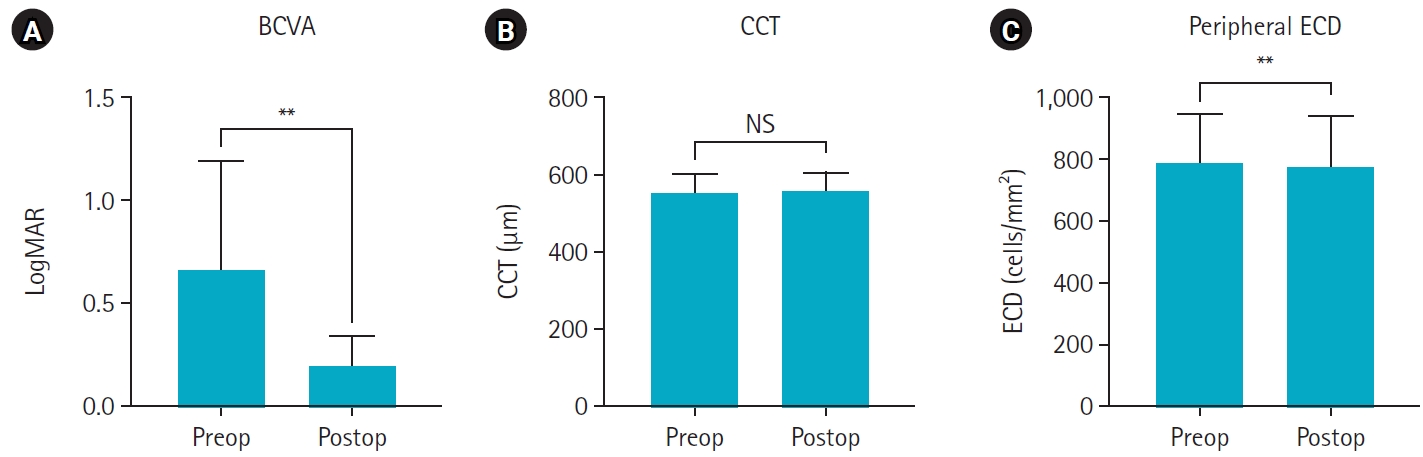
ePub - Purpose
The aim of this study was to analyze the clinical outcomes of cataract surgery in patients with moderate Fuchs endothelial corneal dystrophy (FECD) in whom central endothelial cells could not be observed using specular microscopy.
Methods
This retrospective study included nine eyes in seven patients diagnosed with FECD who underwent phacoemulsification at a single institution between January 2023 and November 2024. A single experienced corneal specialist performed slit-lamp examination and phacoemulsification. Best-corrected visual acuity (BCVA), specular microscopy, and central corneal thickness (CCT) measurements were performed preoperatively and postoperatively, and the outcomes were compared.
Results
The mean age of the patients was 69.8±6.5 years. Three were male patients and four were female patients. The mean preoperative CCT was 559.5±51.8 μm and the mean peripheral endothelial cell density was 599.3±129.4 cells/mm2. BCVA significantly improved in all patients postoperatively, with a mean logMAR BCVA improving from 0.65±0.52 preoperatively to 0.19±0.14 postoperatively (P=0.002). The mean CCT showed no significant change (preoperative, 559.6±51.8 μm; postoperative, 566.8±45.1 μm; P=0.218). In patients with follow-up longer than 6 months, an increase in CCT was observed at 30 days postoperatively, but CCT returned to preoperative levels after 90 days.
Conclusion
In patients with moderate-to-severe FECD in whom central endothelial cells cannot be measured, phacoemulsification may provide favorable visual outcomes if peripheral endothelial cells are observed and corneal edema is absent preoperatively.
- 611 View
- 10 Download

Case Report
- Delayed toxic anterior segment syndrome after cataract surgery: a case report
- Yeoun Sook Chun
- Insights Cataract Refract Surg 2025;10(1):26-31. Published online February 28, 2025
- DOI: https://doi.org/10.63375/icrs.25.005
-
 Abstract
Abstract
 PDF
PDF ePub
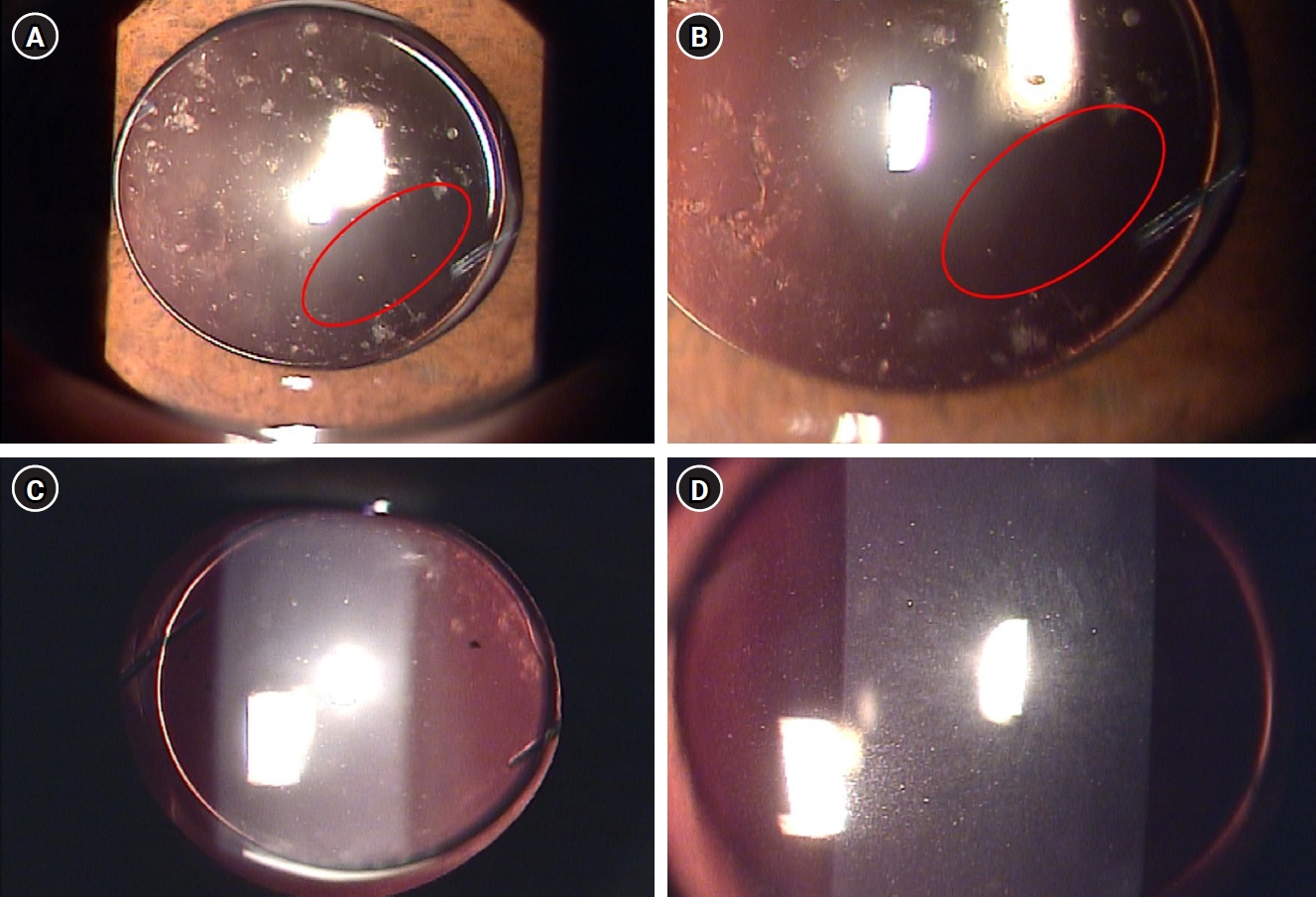
ePub - Purpose
This report describes an unusual case of delayed toxic anterior segment syndrome (TASS) following cataract surgery and its treatment.
Case
summary: A 55-year-old male patient underwent uneventful phacoemulsification with implantation of an intraocular lens (IOL) and eye patching with ophthalmic ointment at the end of the operation. At 1 week postoperatively, a significant increase in the number of anterior chamber inflammatory cells and multiple gray-white deposits on the anterior surface of IOL were noted. All laboratory tests to exclude infectious endophthalmitis were negative. Under the presumptive diagnosis of delayed TASS, an intensive topical steroid was administered. The number of anterior chamber cells decreased; however, the patient complained of blurry vision and multiple whitish precipitates remained on the IOL. Neodymium:yttrium-aluminum-garnet (Nd:YAG) laser treatment was performed to disrupt and remove the precipitates. The deposits were easily and clearly removed using the laser, and there was no recurrence during a 2-year follow-up.
Conclusion
Delayed-onset TASS can manifest as lumpy white inflammatory cell deposits that cannot be controlled with topical steroids. However, Nd:YAG laser treatment can effectively remove inflammatory precipitates.
- 2,244 View
- 27 Download


 KSCRS
KSCRS


 First
First Prev
Prev


