Abstract
-
Purpose
- This report presents a case of diffuse lamellar keratitis (DLK) after femtosecond laser-assisted small incision lenticule extraction (SMILE). The case was presumably associated with meibomian gland dysfunction (MGD).
-
Case summary
- A 25-year-old male patient underwent SMILE surgery. Preoperative examination revealed MGD in both eyes. Despite vigorous cleaning of the eyelid margin and irrigation of the ocular surface, meibomian gland secretion floating on the ocular surface was observed after the lenticule extraction in the right eye. At 2 days postoperatively, stage I DLK was detected. After aggressive topical steroid treatment, the DLK completely resolved without any sequalae.
-
Conclusion
- DLK can occur in association with MGD. Attention should be paid when performing SMILE in eyes with MGD.
-
Keywords: Diffuse lamellar keratitis; Femtosecond laser; Meibomian gland dysfunction; Small incision lenticule extraction
Introduction
Diffuse lamellar keratitis (DLK) is an early complication of lamellar refractive surgery including laser in situ keratomileusis [1,2]. It is characterized by accumulation of non-infectious infiltrates in the corneal lamellar interface [2,3]. The disease can cause symptoms, such as, ocular discomfort, pain, foreign body sensation, photophobia, and visual disturbance [4], although it is not infrequently asymptomatic, particularly in mild cases. Although its pathophysiology is not fully elucidated yet, risk factors including corneal epithelial defect, bacterial endotoxins, surgical debris, chemicals, bleeding, and meibomian gland secretion have been suggested [2,4-10].
DLK can occur in association with any surgery in which corneal lamellar interface is created [9,11], and DLK occurring as a complication of small incision lenticule extraction (SMILE) has been reported with a prevalence of 0.45% to 2.17% [11-13]. The author recently experienced a case of DLK after SMILE that is presumably associated with meibomian gland dysfunction (MGD), thus herein report this case. The patient’s consent form for publication was obtained.
Case Report
A 25-year-old Asian male patient visited our hospital for correction of myopic astigmatism. Past medical history was unremarkable. Best corrected visual acuity (BCVA) was 20/20 in both eyes, and manifest refraction was –5.50=–0.75 at 10° for the right eye and –5.75=–1.00 at 160° for the left eye. Intraocular pressure was 14 mmHg in both eyes by pneumatic applanation tonometry. Central corneal thickness measured using ultrasonic pachymetry (Pacscan 300A; Sonomed Inc.) was 575 μm in the right eye and 565 μm in the left eye.
At the day of the surgery, preoperative anterior segment examination revealed plugging of meibomian gland orifices. Thus, thorough cleaning of eyelid margin and vigorous irrigation of ocular surface was done to remove the meibomian gland secretions.
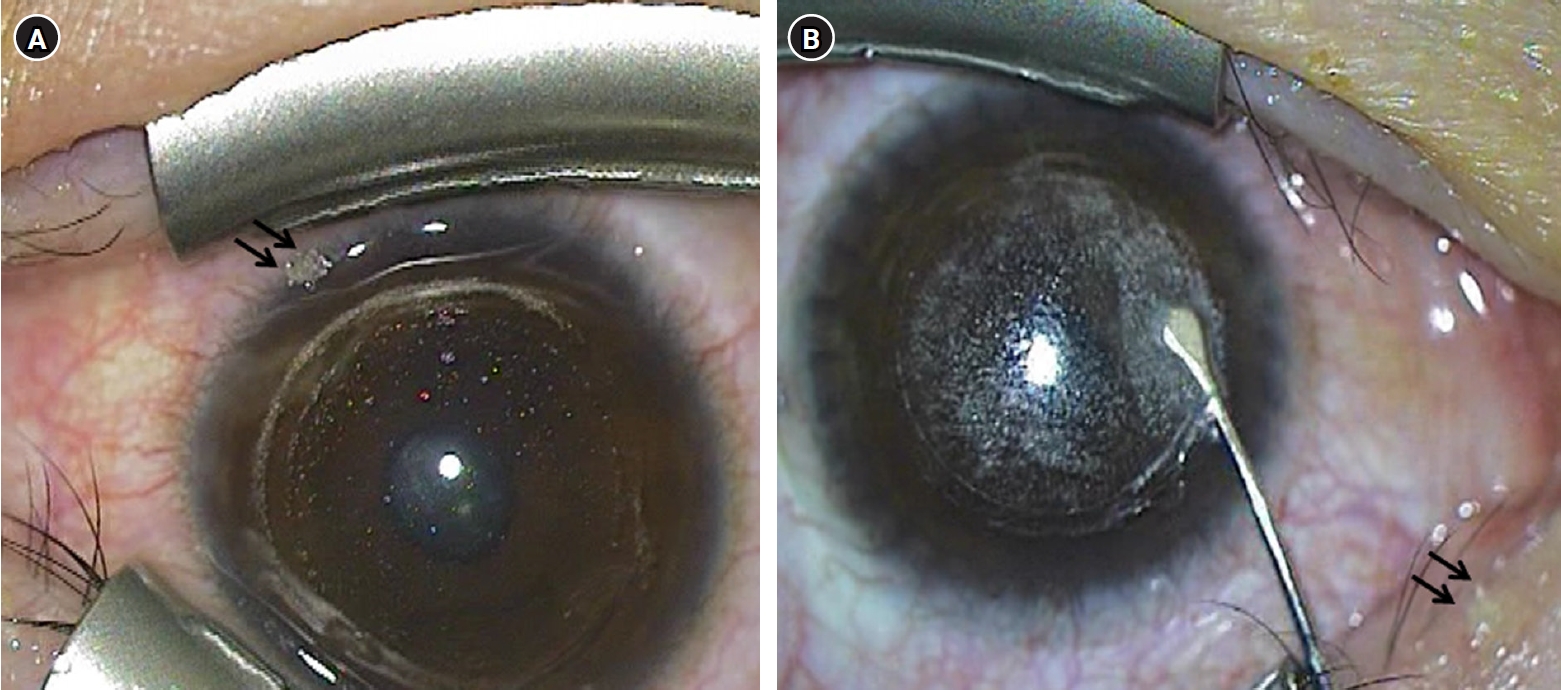
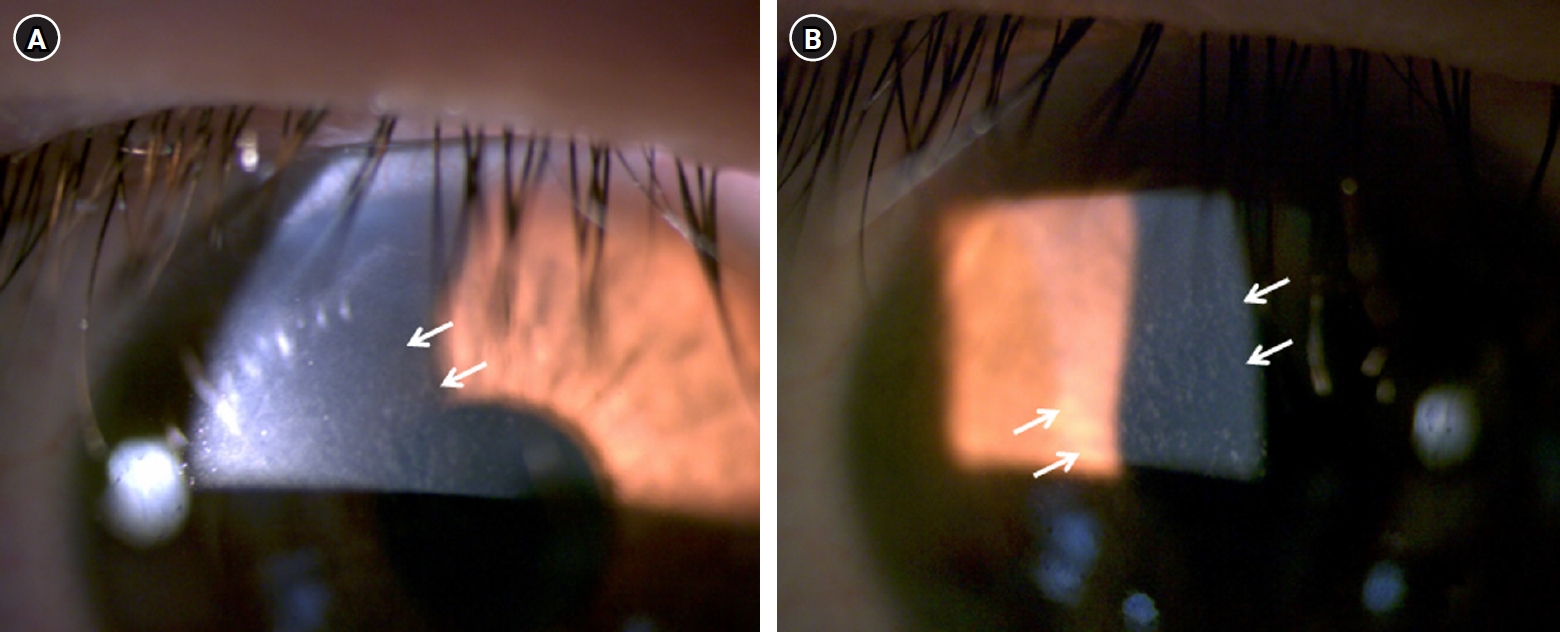
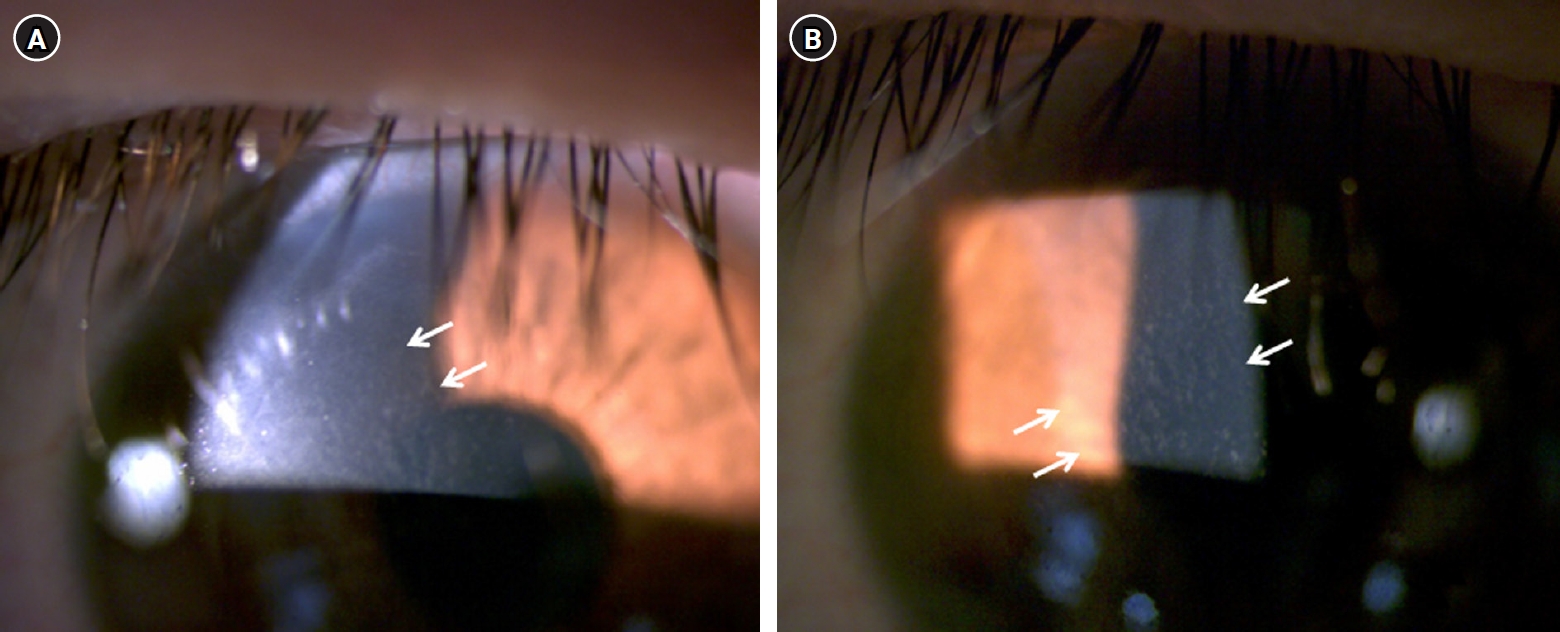
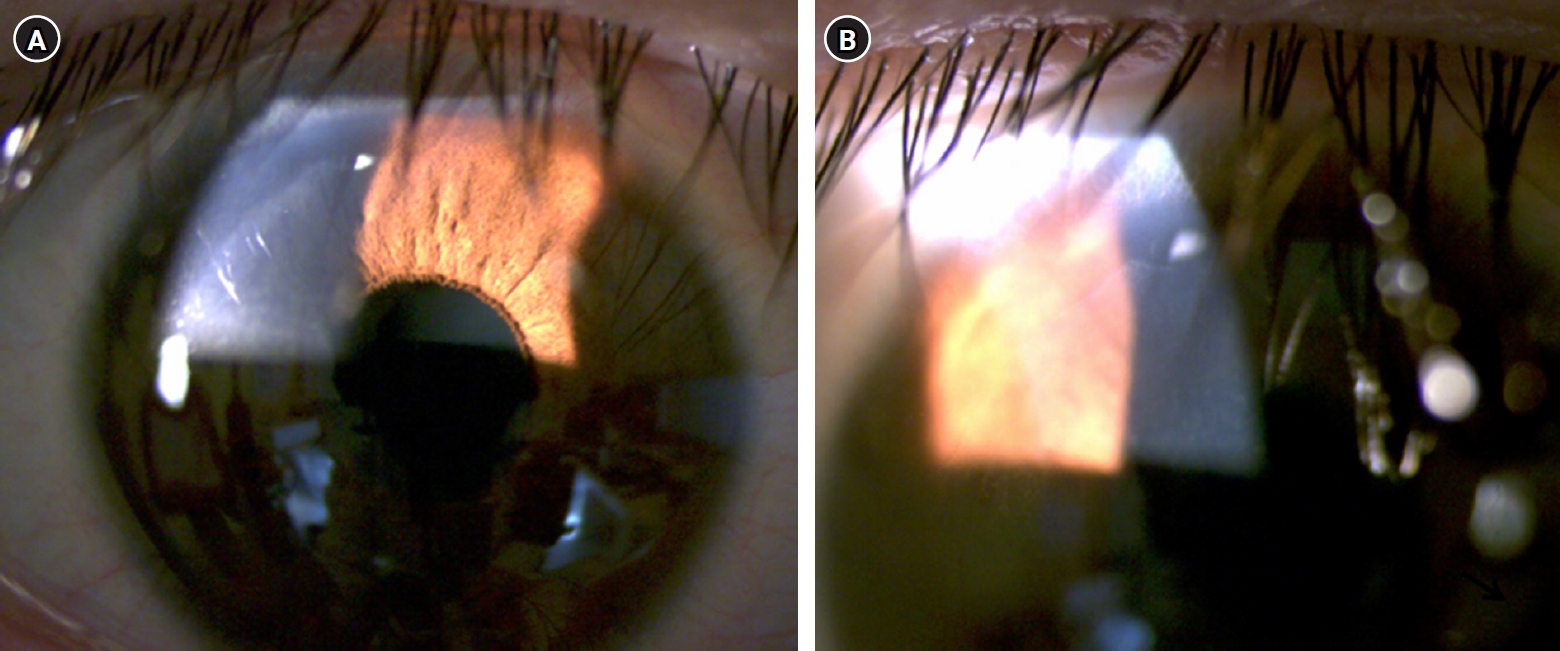
The SMILE surgery was done using a femtosecond laser system (VisuMax; Carl Zeiss Meditec AG) under topical anesthesia with 0.5% proparacaine hydrochloride (Hanmi Pharmaceutical). The cap diameter was 7.5 mm, with a thickness of 130 μm, and the optical zone was 6.5 mm in both eyes. A 3 mm incision was made at 11 o’clock in both eyes. After the uneventful lenticule extraction in the right eye, meibomian gland secretion floating on the ocular surface was found (Fig. 1A). Therefore, vigorous irrigation of the corneal interface and ocular surface was done to prevent contamination with the meibomian gland secretion. Meibomian gland secretion on the upper eyelid was also observed in the left eye during the lenticule separation (Fig. 1B). Because there was a small epithelial defect around the corneal incision in the left eye, bandage contact lens was applied on the left cornea after irrigation of the interface and ocular surface. Postoperative medication consisted of levofloxacin 1.5% (Santen) and fluorometholone 0.1% (Samil Pharmaceutical) four times daily, respectively.
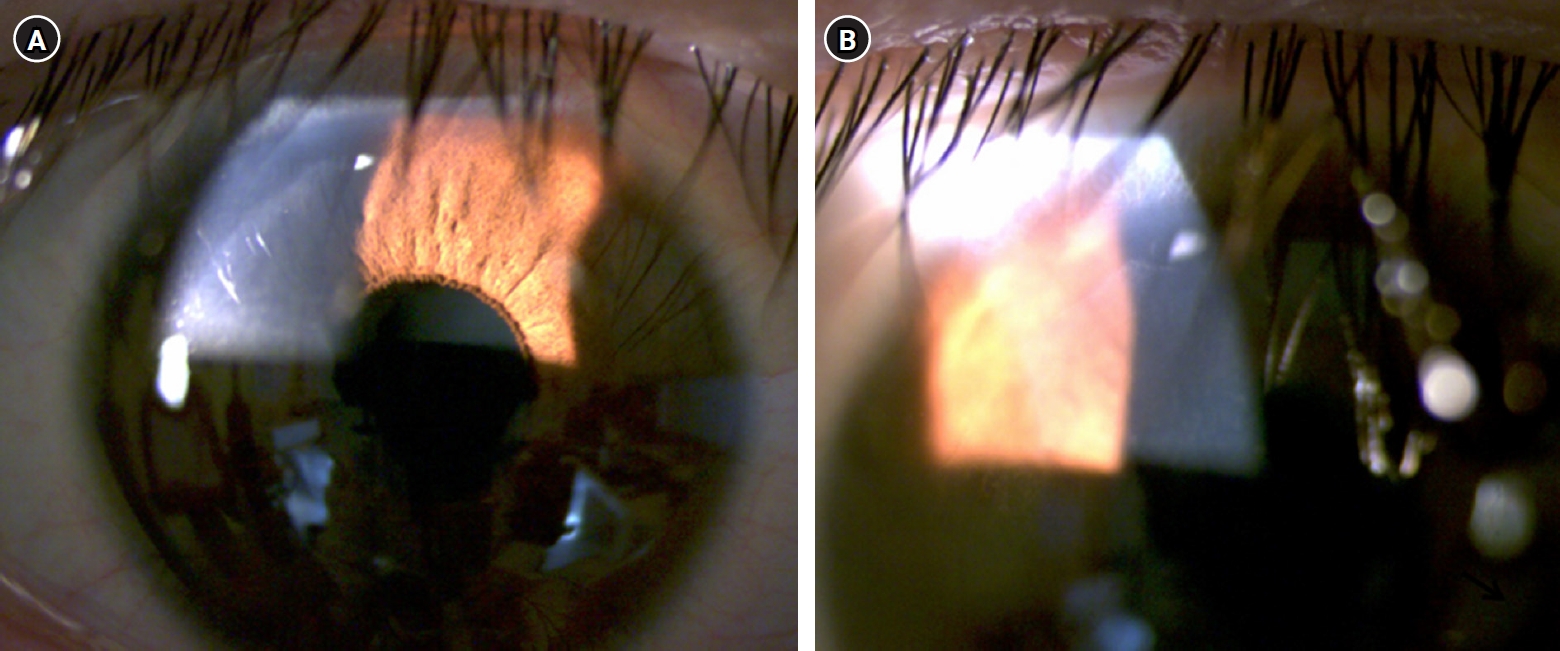
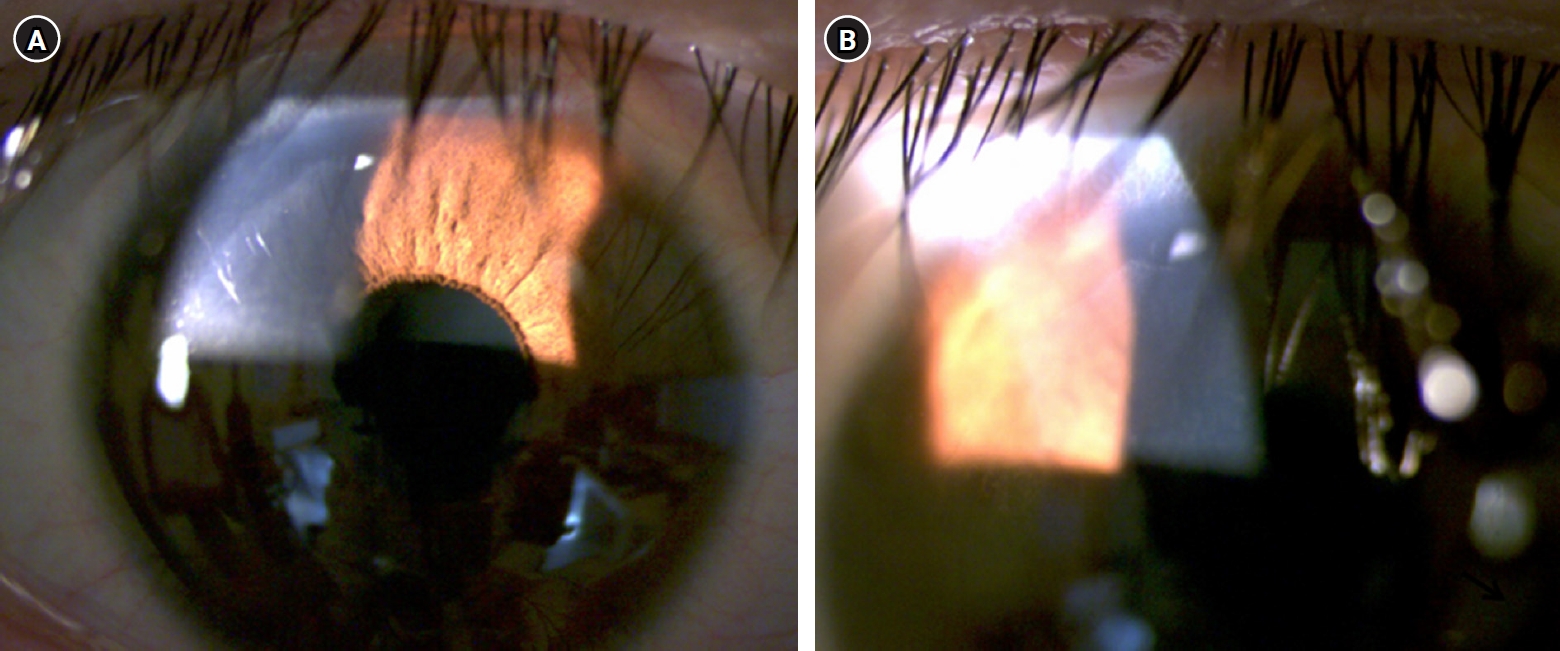
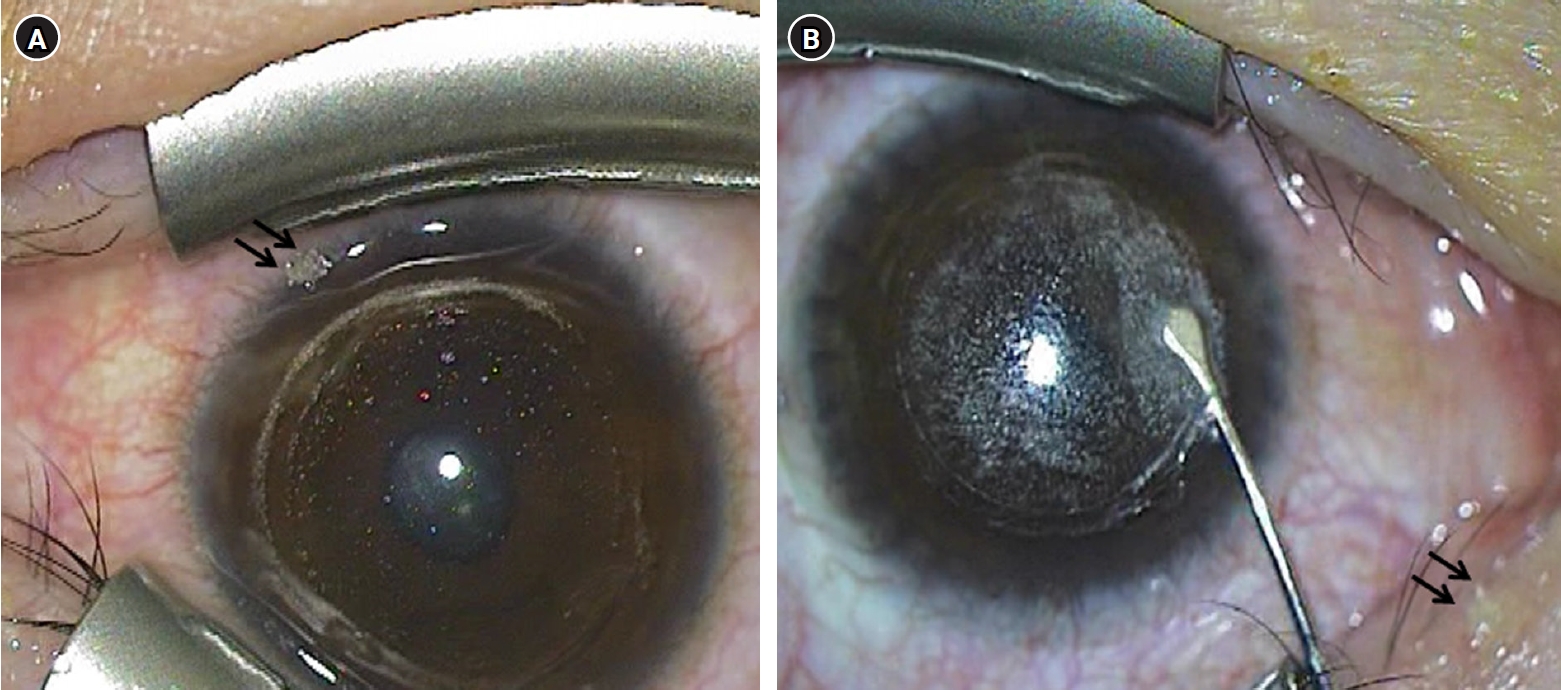
At postoperative 2 days, his BCVA was 20/22 in both eyes and intraocular pressure by applanation tonometry was 11 mmHg in the right eye and 12 mmHg in the left eye. He did not report any symptoms. However, slit lamp examination showed stage I DLK with multiple granular infiltrates in the interface in the right eye (Fig. 2). No infiltrate was observed in the left eye. The dose of fluorometholone 0.1% was increased to eight times daily in the right eye. Three days later, significant improvement of the DLK was found (Fig. 3). One week later, his BCVA was 20/20 in both eyes and the DLK resolved completely without any sequelae. Topical steroid was tapered and stopped two weeks later.
Discussion
To the best of our knowledge, this is the first case report of DLK after SMILE that is presumably associated with MGD. Any other patients who received SMILE procedure in the same batch did not develop MGD, which suggests that the possible other causes, such as, contamination of a sterilizer or instruments with endotoxins, toxicity from chemicals, surgical debris, and talc from gloves can be ruled out [6]. Despite the preoperative cleaning of eyelid and irrigation, the meibomian gland secretion could not be completely removed from the ocular surface, and the remaining meibomian gland secretion might intensify the postoperative recruitment of inflammatory cells and release of inflammatory cytokines and chemokines, which might result in development of MGD [5,6,14]. In addition, MGD could be aggravated after SMILE, which could also lead to introduction of inflammatory mediators into the corneal interface [10,14]. Because the corneal incision was made at 11 o’clock, the inciting agent from the inflamed meibomian glands could directly break into the corneal incision and cause DLK [10]. Although MGD was present in both eyes, DLK developed only in the right eye. It is possibly because the left cornea was covered with bandage contact lens due to the postoperative epithelial defect, which prevented influx of inflammatory material into the corneal incision.
In the present case, DLK responded rapidly to the intensive topical steroid treatment and completely resolved in one week, as reported in previous studies [2,4,10]. It is possibly because the DLK was detected in earlier stage. Studies suggested that aggressive treatment of corneal inflammatory response is mandatory to prevent sequelae, such as, corneal melting, and prompt diagnosis and treatment can result in resolution of DLK without sequelae [2,3,9,15].
In conclusion, attention should be paid to the increased risk of DLK when performing SMILE procedures in eyes with MGD. Preoperative treatment of MGD using warm compression, lid hygiene, and medications, such as, topical antibiotics and steroids can be helpful for the prevention of DLK. Prompt diagnosis and aggressive topical steroid treatment is necessary for good anatomical and visual outcome.
Article Information
Author contributions
All the work was done by SBH.
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
Funding
This paper was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (Grant No. NRF-2021R1F1A1048448).
Data availability
Not applicable.
Fig. 1.Still images of the intraoperative videos. (A) Meibomian gland secretion (arrows) floating on the ocular surface was detected after the lenticule extraction in the right eye. (B) Meibomian gland secretion (arrows) on the upper eyelid was visible in the left eye during lenticule separation.
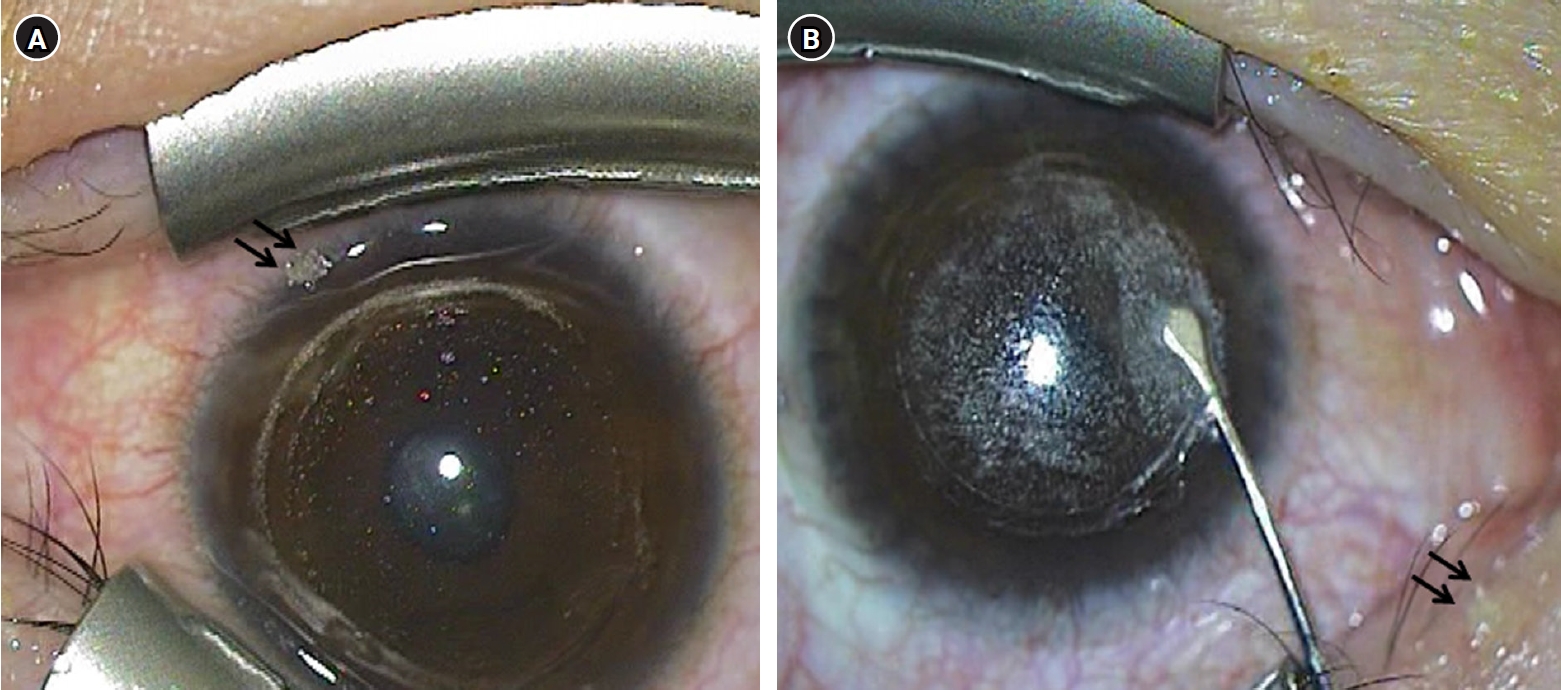
Fig. 2.Anterior segment photographs at the second day after surgery. (A, B) Stage I diffuse lamellar keratitis with multiple granular infiltrates (arrows) was observed at the interface in the right eye.
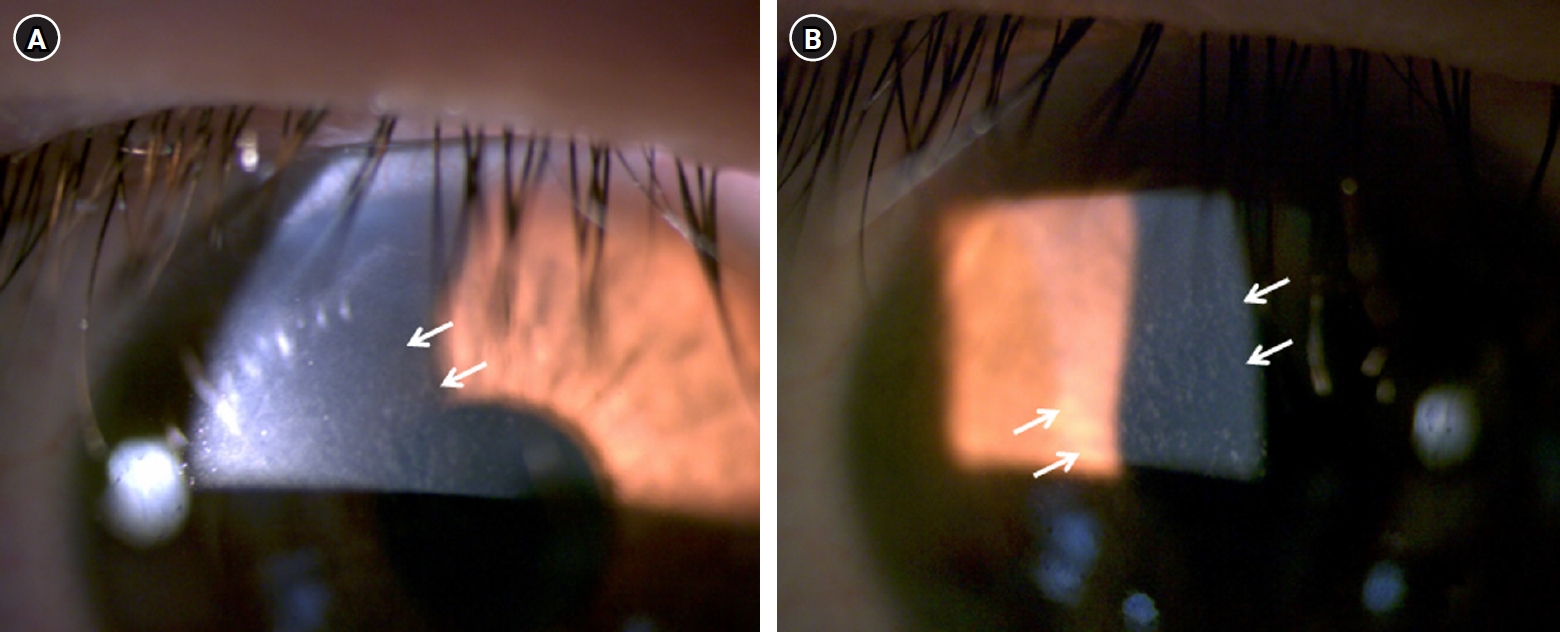
Fig. 3.Anterior segment photographs at the fifth day after surgery. (A, B) Improvement in diffuse lamellar keratitis can be observed at the corneal interface.
References
- 1. Smith RJ, Maloney RK. Diffuse lamellar keratitis: a new syndrome in lamellar refractive surgery. Ophthalmology 1998;105:1721‒6. ArticlePubMed
- 2. Kymionis GD, Tsoulnaras KI, Tsakalis NG, Grentzelos MA. Diffuse lamellar keratitis in the femtosecond-assisted LASIK flap tunnel. Clin Ophthalmol 2014;8:1065‒7. ArticlePubMedPMC
- 3. Linebarger EJ, Hardten DR, Lindstrom RL. Diffuse lamellar keratitis: diagnosis and management. J Cataract Refract Surg 2000;26:1072‒7. ArticlePubMed
- 4. Labani S, Basli E, Goemaere I, et al. Atypical severe diffuse lamellar keratitis presenting as concentric rings after femtosecond laser-assisted small-incision lenticule extraction (SMILE). J Fr Ophtalmol 2020;43:e95‒9. ArticlePubMed
- 5. Wilson SE, de Oliveira RC. Pathophysiology and treatment of diffuse lamellar keratitis. J Refract Surg 2020;36:124‒30. ArticlePubMed
- 6. Yuan M, Ji R, Zhang R. A case of severe diffuse lamellar keratitis after small-incision lenticule extraction operation. Indian J Ophthalmol 2024;72:1219‒23. ArticlePubMedPMC
- 7. Alqahtani SS. A case report of diffuse lamellar keratitis after femtoSMILE refractive surgery. Case Rep Ophthalmol 2020;11:582‒7. ArticlePubMedPMCPDF
- 8. Ambrósio R Jr, Periman LM, Netto MV, Wilson SE. Bilateral marginal sterile infiltrates and diffuse lamellar keratitis after laser in situ keratomileusis. J Refract Surg 2003;19:154‒8. ArticlePubMed
- 9. Balestrazzi A, Balestrazzi A, Giannico MI, et al. Diagnosis, clinical trend, and treatment of diffuse lamellar keratitis after femtosecond laser-assisted in situ keratomileusis: a case report. Case Rep Ophthalmol 2018;9:457‒64. ArticlePubMedPMCPDF
- 10. Fogla R, Rao SK, Padmanabhan P. Diffuse lamellar keratitis: are meibomian secretions responsible? J Cataract Refract Surg 2001;27:493‒5. ArticlePubMed
- 11. Zhao J, He L, Yao P, et al. Diffuse lamellar keratitis after small-incision lenticule extraction. J Cataract Refract Surg 2015;41:400‒7. ArticlePubMed
- 12. Reinstein DZ, Stuart AJ, Vida RS, et al. Incidence and outcomes of sterile multifocal inflammatory keratitis and diffuse lamellar keratitis after SMILE. J Refract Surg 2018;34:751‒9. ArticlePubMed
- 13. Wang Y, Ma J, Zhang L, et al. Postoperative corneal complications in small incision lenticule extraction: long-term study. J Refract Surg 2019;35:146‒52. ArticlePubMed
- 14. Suzuki T. Inflamed obstructive meibomian gland dysfunction causes ocular surface inflammation. Invest Ophthalmol Vis Sci 2018;59:DES94‒101. ArticlePubMed
- 15. Moshirfar M, Zhang S, Pandya S, et al. Incidence and Management of epithelial-related complications after SMILE. Clin Ophthalmol 2023;17:2777‒89. ArticlePubMedPMCPDF
Citations
Citations to this article as recorded by




 KSCRS
KSCRS
 ePub Link
ePub Link Cite
Cite

