Previous issues
- Page Path
- HOME > Browse articles > Previous issues
Review Articles
- Current updates in the treatment of keratoconus
- Mee Kum Kim
- Insights Cataract Refract Surg 2025;10(2):33-41. Published online June 30, 2025
- DOI: https://doi.org/10.63375/icrs.25.010
-
 Abstract
Abstract
 PDF
PDF ePub
ePub - Corneal collagen cross-linking is a primary treatment to slow or halt the progression of keratoconus. For visual rehabilitation, important treatments include contact lenses fitting, intracorneal ring segment implantation, and corneal transplantation. Additionally, either phakic intraocular lenses or corneal therapeutic keratectomy combined with corneal collagen cross-linking can assist in visual rehabilitation with limited indications. New methods for visual rehabilitation, such as stromal keratophakia, have been introduced. This review evaluates and compares the efficacy and safety of various treatments for keratoconus based on the latest information.
- 851 View
- 18 Download

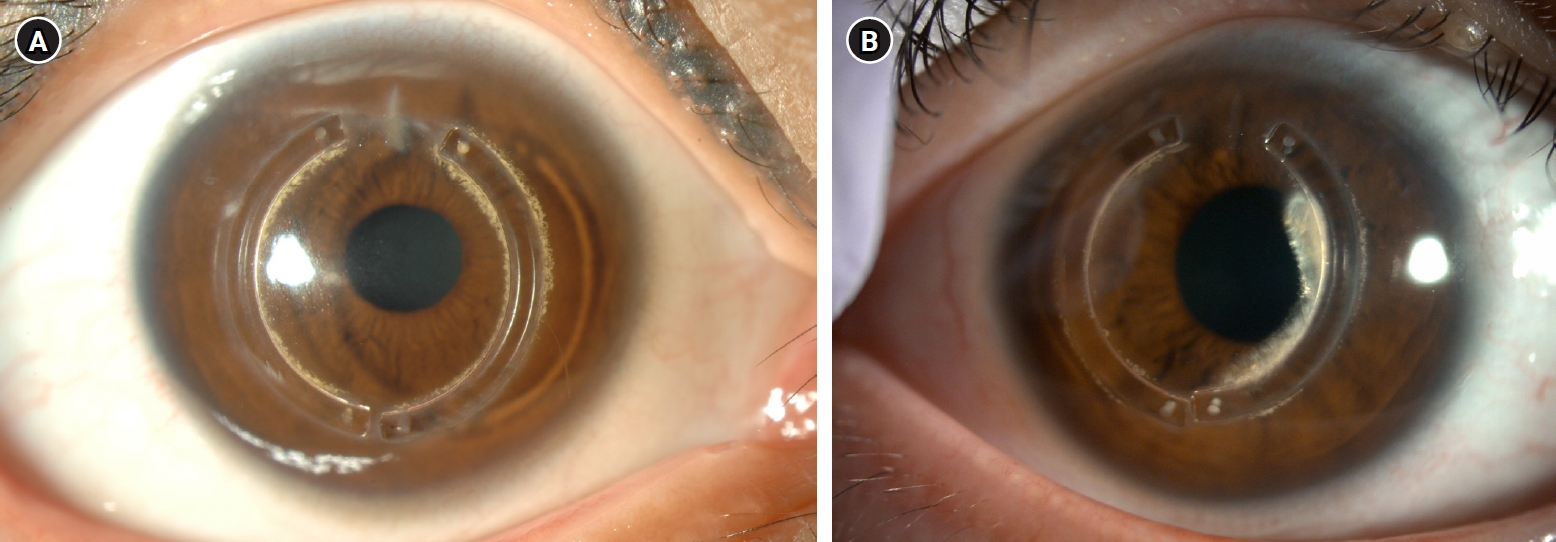
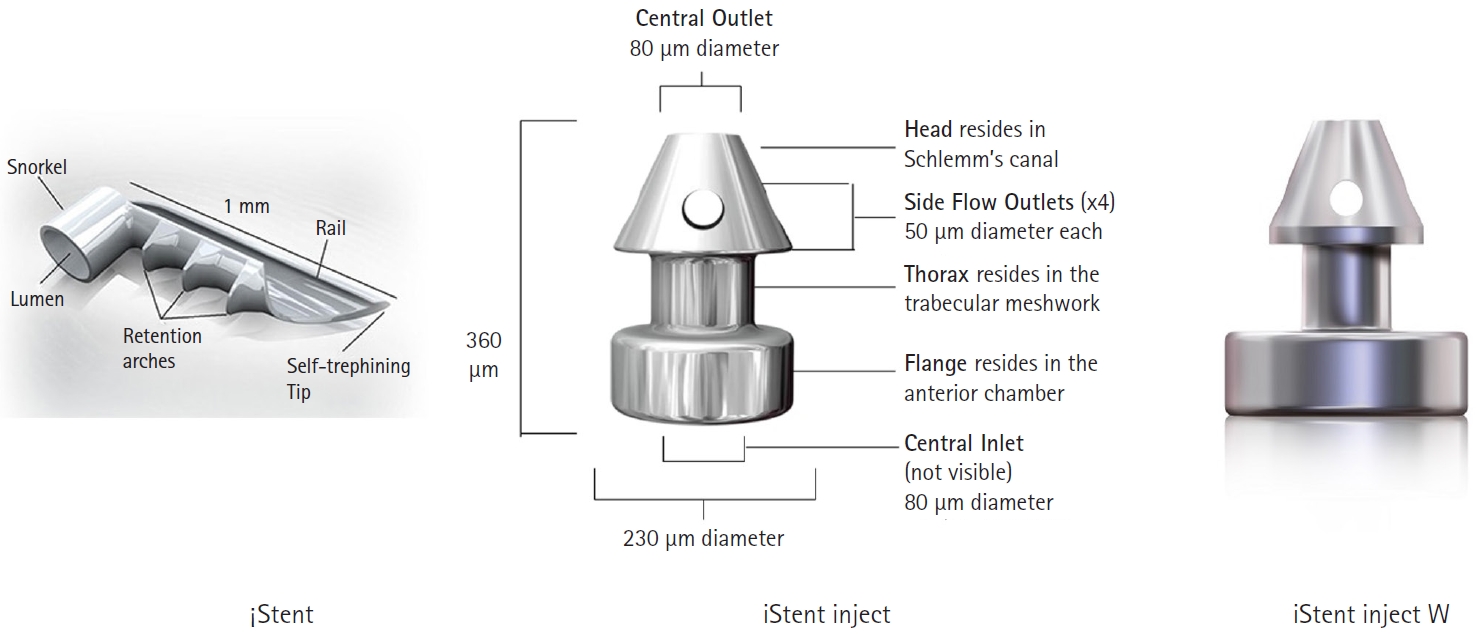
- Trabecular microbypass using iStent combined with cataract surgery
- Yeoun Sook Chun
- Insights Cataract Refract Surg 2025;10(2):42-51. Published online June 30, 2025
- DOI: https://doi.org/10.63375/icrs.25.007
-
 Abstract
Abstract
 PDF
PDF ePub
ePub - Minimally invasive glaucoma surgery has revolutionized conventional glaucoma treatment due to its simple procedures, rapid recovery, and few complications. iStent, a trabecular microbypass that can be implanted via combined cataract surgery, has the advantage of lowering intraocular pressure (IOP) independent of bleb formation. Furthermore, it is straightforward to implement and does not involve a substantial burden. iStent has a synergetic effect with phacoemulsification. Combining iStent with phacoemulsification yielded a greater reduction of IOP and glaucoma eyedrops, as well as higher rates of visual field change, than when either modality was used in isolation. iStent has emerged as a new treatment option for patients with mild to moderate glaucoma. This review aims to improve readers’ understanding of iStent by summarizing the surgical techniques needed to correctly insert it for optimal outcomes and discussing problem-solving in the context of patient care.
- 732 View
- 9 Download

Original Article
- Efficacy of extended depth of focus, enhanced monofocal, and monofocal intraocular lenses in patients with retinal disease
- Eun Chul Kim
- Insights Cataract Refract Surg 2025;10(2):52-60. Published online June 30, 2025
- DOI: https://doi.org/10.63375/icrs.25.009
-
 Abstract
Abstract
 PDF
PDF ePub
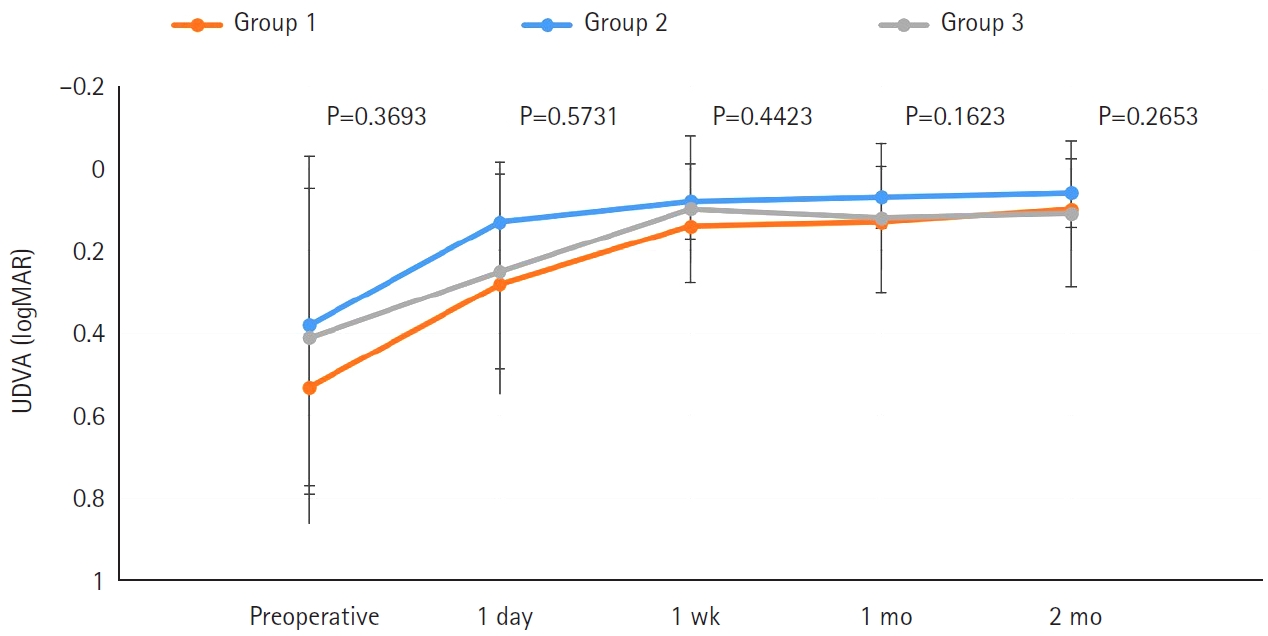
ePub - Purpose
The aim of this study was to compare the visual quality of extended depth of focus (EDOF), enhanced monofocal, and monofocal intraocular lenses (IOLs) in patients with retinal disease.
Methods
In total, 103 eyes from 93 patients (group 1: enhanced monofocal ICB00, n=36; group 2: EDOF ZXR00, n=36; group 3: monofocal ZCB00, n=31) were retrospectively enrolled. Uncorrected and corrected near visual acuity (UNVA, CNVA), intermediate visual acuity (UIVA, CIVA), and distance visual acuity (UDVA, CDVA), manifest refraction spherical equivalent (MRSE), and satisfaction scores were assessed before and after surgery.
Results
The postoperative UDVA, CDVA, and MRSE of the three groups were better than the preoperative data, respectively (P<0.05). The UIVA of group 1 (0.13±0.12 logMAR) and 2 (0.10±0.11) was significantly better than that of groups 3 (0.25±0.15) (P<0.05). The UNVA of group 2 (0.18±0.12) was significantly better than that of groups 1 (0.32±0.20) and 3 (0.45±0.26; P<0.05). The UDVA of patients with macular edema and macular holes was insignificantly lower than that of epiretinal membranes and high myopia. The overall satisfaction of group 1 (1.58±0.81) and 2 (1.46±0.75) was significantly better than that of groups 3 (1.83±0.97; P<0.05).
Conclusion
EDOF and enhanced monofocal IOLs were associated with better intermediate and near vision than monofocal IOLs in patients with retinal disease. However, monofocal IOLs are recommended in patients with macular edema and macular holes, unlike patients with epiretinal membranes and high myopia.
- 835 View
- 18 Download

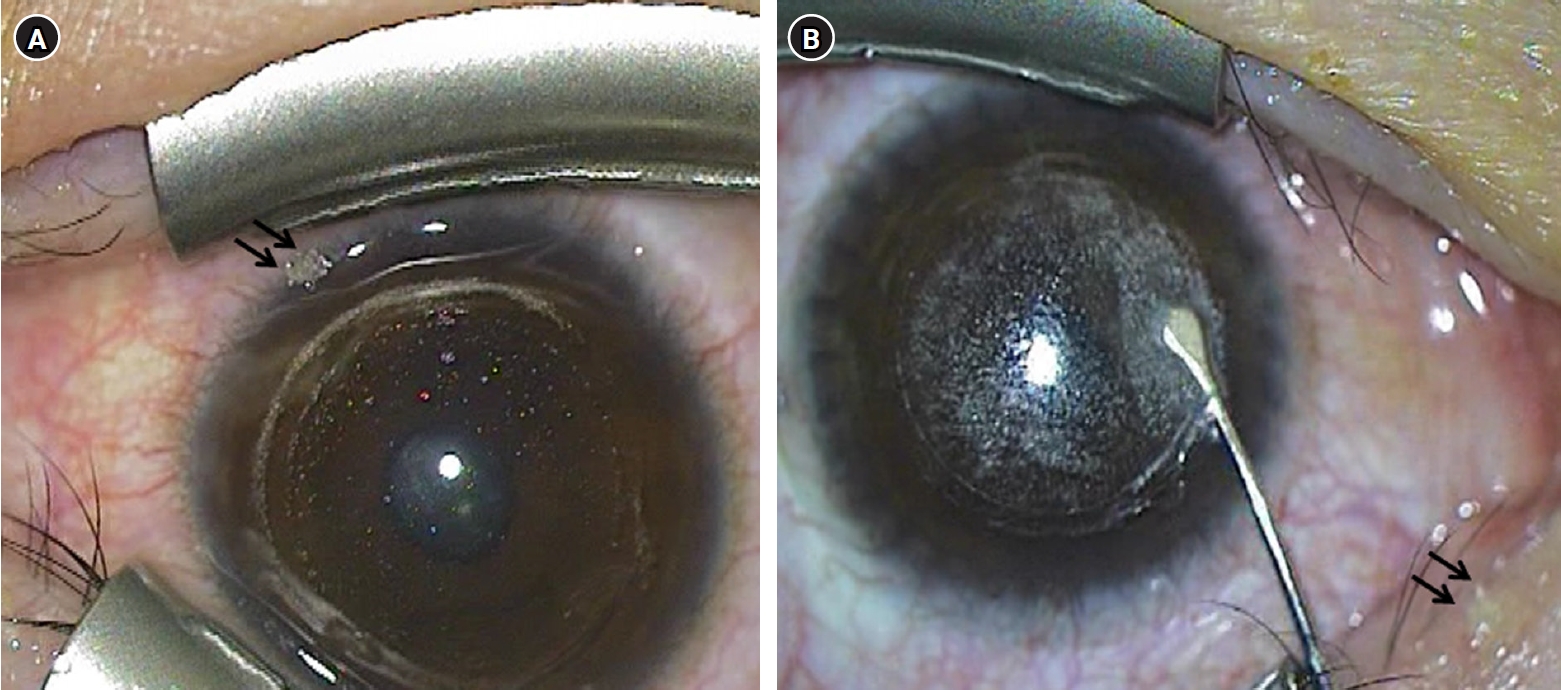
Case Report
- Diffuse lamellar keratitis after small incision lenticule extraction: presumably related to meibomian gland dysfunction
- Sang Beom Han
- Insights Cataract Refract Surg 2025;10(2):61-64. Published online June 30, 2025
- DOI: https://doi.org/10.63375/icrs.25.008
-
 Abstract
Abstract
 PDF
PDF ePub
ePub - Purpose
This report presents a case of diffuse lamellar keratitis (DLK) after femtosecond laser-assisted small incision lenticule extraction (SMILE). The case was presumably associated with meibomian gland dysfunction (MGD).
Case
summary: A 25-year-old male patient underwent SMILE surgery. Preoperative examination revealed MGD in both eyes. Despite vigorous cleaning of the eyelid margin and irrigation of the ocular surface, meibomian gland secretion floating on the ocular surface was observed after the lenticule extraction in the right eye. At 2 days postoperatively, stage I DLK was detected. After aggressive topical steroid treatment, the DLK completely resolved without any sequalae.
Conclusion
DLK can occur in association with MGD. Attention should be paid when performing SMILE in eyes with MGD.
- 2,020 View
- 16 Download


 KSCRS
KSCRS


 First
First Prev
Prev


